Understanding Body Mass Index (BMI): A Comprehensive Guide
What is BMI?
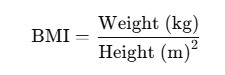
The Body Mass Index (BMI) is a statistical measure designed to evaluate the relationship between an individual’s weight and height. Developed by Belgian polymath Adolphe Quetelet between 1830 and 1850 as part of his “social physics” framework, it is also known as the Quetelet Index. BMI is calculated using these formulas:
Metric Formula:
Imperial Formula:
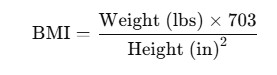
These simple calculations make BMI accessible to anyone, enabling both researchers and individuals to estimate weight-related health risks.
BMI – A Statistical Tool
BMI serves as a public health tool that allows researchers to analyze large datasets where height and weight are recorded. It helps identify trends and correlations between body weight and health outcomes, such as obesity-related conditions. While BMI does not directly measure body fat, its simplicity and universal adoption make it invaluable for global health studies.
Limitations of BMI
Despite its utility, BMI has notable limitations:
- It is not a direct measure of body fat. For example, a muscular individual, such as a bodybuilder, may have a high BMI without excess body fat.
- It does not account for body composition differences. Elderly individuals with low muscle and bone mass may appear within a “normal” BMI range but still have excessive fat.
- It overlooks individual differences. Ethnicity, gender, and age can affect how BMI relates to health risks.
Practical Uses of BMI
- Public Health and Research:
- BMI has been a key measure for defining obesity in public health initiatives worldwide since the 1980s.
- It is the standard for the World Health Organization’s (WHO) obesity statistics.
- Personal Health Assessments:
- Governments and organizations have popularized BMI as an easy, at-home method to estimate whether an individual is underweight, at an optimal weight, overweight, or obese.
- However, tools like skinfold thickness tests or bioelectrical impedance are more accurate for clinical diagnostics.
- Children and Adolescents:
- BMI for children (ages 2–20) is calculated the same way but interpreted differently. Instead of fixed thresholds, it uses percentiles:
- Underweight: Less than the 5th percentile
- Overweight: Above the 95th percentile
- At risk of overweight: 85th–95th percentile
- BMI for children (ages 2–20) is calculated the same way but interpreted differently. Instead of fixed thresholds, it uses percentiles:
BMI Categories and Thresholds
BMI values are categorized to simplify their interpretation:
| Category | BMI Range |
|---|---|
| Underweight | <18.5 |
| Normal weight | 18.5–24.9 |
| Overweight | 25–29.9 |
| Obese | 30–39.9 |
| Extremely obese | ≥40 |
Global and Ethnic Considerations
BMI thresholds are not universal. For instance:
- The WHO recommends a lower overweight threshold for South East Asians, with BMI values above 23 considered overweight and above 25 classified as obese.
- These adjustments acknowledge differences in body composition across ethnic groups, with further revisions expected as clinical studies progress.
Historical Shifts in BMI Standards
In 1998, the U.S. National Institutes of Health (NIH) lowered the threshold for overweight from 27.8 to 25 to align with WHO guidelines. This reclassification increased the number of Americans classified as overweight by approximately 30 million.
BMI in Context
BMI should be seen as one of several tools for understanding weight and health:
- Extreme Cases: In cases of severe underweight or obesity, BMI is less relevant, as visual assessments or more detailed diagnostics (e.g., bioelectrical impedance) are sufficient.
- Population Trends: BMI remains a valuable indicator for public health studies and monitoring trends in obesity and undernutrition across populations.
Conclusion
The Body Mass Index offers a broad, accessible method for estimating weight-related health risks but should not be used in isolation for individual diagnoses. Its effectiveness lies in population-level studies, with alternative measures recommended for clinical assessments. While BMI has its limitations, its simplicity and global adoption ensure it remains an essential tool in public health, particularly when combined with more nuanced diagnostic methods.






